Usted está aquí
Peruvian Journal of Neurosurgery
Selective posterior corpus callosotomy in a child with Lennox–Gastaut Syndrome: case report
ZINDYA BARRIENTOS M., MARCO MEJÍA T., FERNANDO PALACIOS S.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
Introduction: In epilepsy refractory to medical treatment which presents multiple and bilateral epileptogenic foci such as Lennox Gastaut syndrome (LGS) the surgical alternative is disconnection surgery such as callosotomy. Posterior callosotomy is indicated in cases of atonic seizures with posterior resection, leading to better seizure control especially when resection surgeries of the anterior third or anterior two-thirds of the corpus callosum fail. We present the case of a patient with Lennox Gastaut syndrome who required a posterior callosotomy after a partial anterior callosotomy, finally achieving complete control of atonic seizures.
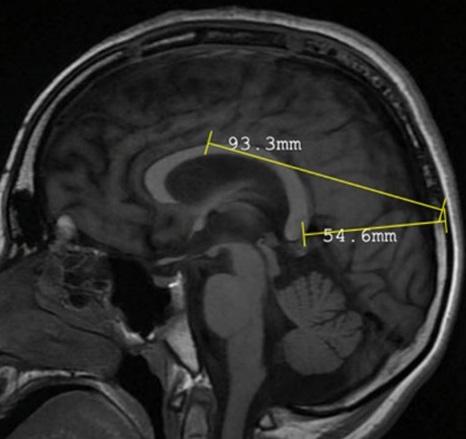
Clinical case: a 10-year-old male patient with a diagnosis of drug-resistant epilepsy due to Lennox Gastaut syndrome, and a surgical history of a partial callosotomy of the anterior third of the corpus callosum. In March 2021 which achieved only a transient decrease in seizures. The patient had had atonic seizures for 6 years and had been unsuccessfully treated with 5 different anticonvulsant medications such as topiramate clonazepam levetiracetam lamotrigine and valproate. On examination: Awake, alert, moderate to severe psychomotor retardation. Brain MRI was normal. A posterior microsurgical callosotomy was performed without complications. His postoperative clinical evolution was favorable showing an absence of atonic seizures.
Conclusions: Selective posterior callosotomy is an essential tool in controlling seizures in cases of refractory epilepsy in patients with atonic seizures. Our study suggests that posterior callosotomy is likely to be even more effective and safe when resections of different segments of the corpus callosum are combined.
Keywords: Corpus Callosum, Seizures, Lennox Gastaut Syndrome, Drug Resistant Epilepsy. (Source: MeSH NLM)