Injured glioma syndrome: report of a case with unfavorable outcome
DANILO ZAVALAGA N., ERMITAÑO BAUTISTA C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish)
ABSTRACT
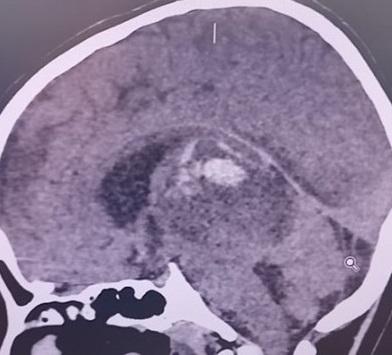
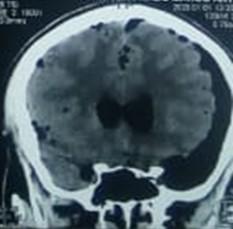
Introduction: Wounded Glioma Syndrome (WGS) is a clinical picture described after resection of high-grade tumors. It is characterized by the presence of hemorrhage and postoperative edema that is difficult to manage, leading to significant sequelae and in some cases death. Pre and postoperative conditions play an important role in WGS, as well as factors related to surgery such as modification of tumor and peritumoral blood flow, altered coagulation, among others.
Clinical case: 12-year-old patient with a diagnosis of anaplastic astrocytoma who underwent partial surgical resection, without presenting complications. At 48 hours, the patient presented clinical signs of intracranial hypertension, the brain tomography revealed bleeding in the surgical bed and significant perilesional edema. Barbiturate coma, neuroprotective measures, and anti-edema treatment were induced. The patient remained in the ICU for 23 days, leaving the ICU on a 5-point Glasgow Coma Scale, dependent on mechanical ventilation so far.
Conclusion: This case shows the rapid deterioration and important sequelae that a patient with glioma surgery can present. Complete resection is not always possible. Therefore, when faced with incomplete resection or a biopsy, neurosurgeons must consider this syndrome, as well as its implications and repercussions in the immediate postoperative period; To assess the risk/benefit when planning surgery and act early, if this syndrome occurs.
Keywords: Glioma, Astrocytoma, Hemorrhage, Edema, Intracranial Hypertension, (Source: MeSH NLM)
Aesthetic and psychological outcomes of cranioplasty, polymethyl methacrylate versus titanium mesh
ESSAM M. YOUSSEF, MD, DINA A. SELEEM, MD, MOHAMED A. YAHIA, MD
Abstract (Spanish) ||
Full Text ||
PDF (English)
ABSTRACT
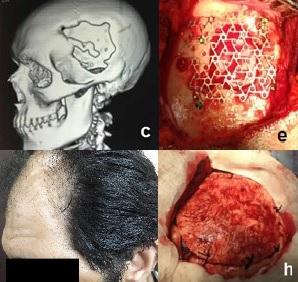
Introduction: Problems with appearance may negatively affect the mental health of individuals with disfigurement so, cranioplasty has an important role in improving the physical appearance of patients as well as their psychological symptoms.
Objective: This study aims to highlight the aesthetic as well as the psychological outcomes of cranioplasty using the two most widely used synthetic graft materials; polymethyl methacrylate (PMMA) and titanium mesh.
Methods: This is a prospective study conducted on patients with apparent skull deformity who underwent cranioplasty using PMMA or titanium mesh from April 2016 to April 2017 and were followed up for one year. Patients were assessed preoperatively, at three months, and one year postoperatively using the Derriford Appearance Scale 24 (DAS 24) and the Hospital Anxiety and Depression scale (HADS).
Results: 42 patients; 25 males and 17 females were recruited. PMMA was used in 23 patients while titanium mesh was used in 19 patients. There were no significant differences regarding early and late complications between both groups. Revision surgery was necessary in only four cases having equal rates between both groups. There was a marked reduction in DAS 24 and HADS scores postoperatively with better scores in the PMMA group especially at three months after cranioplasty.
Conclusion: Cranioplasty had positive effects on patients' distress regarding their appearance and their psychological symptoms. PMMA had better parameters than titanium mesh. Both PMMA and titanium mesh had comparable aesthetic outcomes with no statistically significant difference regarding the complication rates.
Keywords: Cranioplasty, Polymethyl methacrylate, Titanium, Physical Appearance, Body, Depression (source: MeSH NLM)
Impact of the COVID-19 pandemic on patients with rupture of intracranial aneurysm at the Dos de Mayo National Hospital in Lima Peru
JOSÉ LUIS ACHA S., JULIO JOSYMAR QUISPE D.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
|
Objective: To evaluate the impact on the outcome of patients with a ruptured aneurysm, who are admitted to the Dos de Mayo National Hospital in the context of the COVID-19 pandemic.
Methods: 42 operated for ruptured aneurysms were included in the context of the COVID-19 pandemic between March 1 and December 31, 2020 (group A), and a control group of 44 patients operated on between March 1 and December 31, 2019 (group B). Upon admission, the poor neurological status defined by the WFNS> 3, the Fisher IV high-grade tomographic status with intracerebral hematoma or acute hydrocephalus, which required external ventricular drainage (EVD), and the presence of vasospasm were evaluated. The Modified Rankin Scale was evaluated at discharge. Statistical analysis was performed to compare both groups.
Results: The rates of poor neurological presentation and complications during the presurgical evolution (intracerebral hemorrhage and acute hydrocephalus that required EVD) were higher in group A (p = 0.002 and p <0.05, respectively). The delay in the admission of the patient to the emergency room to receive treatment was 7.5 days in group A and 4.95 days for group B. All these factors contributed to a lower possibility of recovery in group A, which was correlated with higher Values on the Modified Rankin Scale at discharge for this group (p = 0.04).
Conclusion: We did not find national reports on ruptured aneurysms treated in the context of the pandemic, this being one of the first studies that demonstrate the impact of the COVID-19 pandemic in patients with ruptured intracranial aneurysm. The population should be educated on how to act in case of specific symptoms such as sudden intense headache, neurological deficit, or acute chest pain, which should receive timely care, immediate referral, and priority of treatment in referral hospitals in order to reduce morbidity and mortality of complex neurological pathologies.
Keywords: Intracranial Aneurysm, Aneurysm, Ruptured, Cerebral Hemorrhage, Pandemics, COVID-19. (Source: MeSH NLM)
|
Mild cranioencephalic trauma in the child population. Experience at the Baca Ortiz Hospital, Quito-Ecuador, 2016-2019
ANDREA PAEZ T., ALICIA TORRES M., ADRIANA GONZÁLEZ G., RODOLFO BERNAL C., JESÚS CASTRO V.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
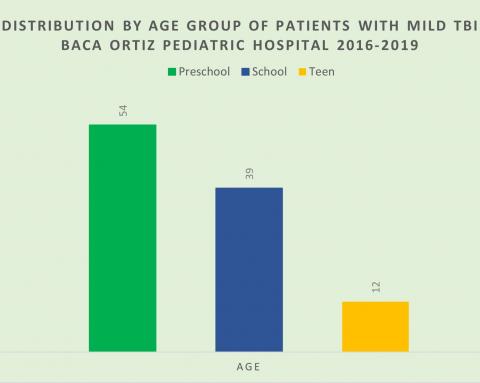
Introduction: The alteration at the anatomical and/or functional level, both motors, sensory and cognitive, a product of the sudden exchange of mechanical energy caused by an external force on the skull, is what defines a traumatic brain injury (TBI). The permanence or transience of these alterations determines the severity of the TBI, with 70 to 80% of a mild type whose neurological symptoms are of little intensity and duration. Clinical observation in mild TBI includes observing children under 2 years of age with trauma without fracture or admission criteria clinically for 2 to 4 hours and observing children with symptoms or mechanism of fall for 4 to 6 hours not known. The objective of the study is to describe mild TBI at Baca Ortiz Pediatric Hospital, a national children's referral hospital in Ecuador, during the period from January 2016 to December 2019.
Methods: Cross-sectional, descriptive, and retrospective study that includes patients diagnosed with mild head trauma evaluated and treated in the Neurosurgery Service of the Baca Ortiz Pediatric Hospital, from January 2016 to December 2019.
Results: During the period 2016 to 2019, 105 children with mild TBI were diagnosed and treated, this being more frequent in males (62.85%) and during the preschool stage (51.42%). Of all of them, 82.85% received specialty medical care in the first 6 hours after the trauma. The main etiology was the fall produced at home (66.66%).
Conclusions: Mild traumatic brain injury is one of the main reasons for pediatric hospital consultation in our setting. It mostly occurs in male patients of preschool age, because of falls at home.
Keywords: Craniocerebral Trauma, Child, Hospitals, Pediatric, Referral and Consultation (Source: MeSH NLM)
Neurological Severity Classification System (CSN-System) in adults with BTI, Hospital Cayetano Heredia, Lima - Peru, 2020. Preliminary study
ELDER CASTRO C., ROMULO RODRIGUEZ C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Objectives: Traumatic Brain Injury (TBI) is the disruption of brain function and architecture. The Glasgow Coma Scale (GCS) is the most widely used TBI severity classification; however, it assesses the functional status of the brain resulting from highly heterogeneous lesions and has little accuracy. The Neurological Severity Classification System (NSC System), a clinical-tomographic instrument designed to overcome lesion heterogeneity, assesses brain function and structure in determining the severity of BTI.
Methods: Observational, prospective, and cross-sectional study in adults with BTI from the emergency service of the Cayetano Heredia Hospital, April - August 2020. It included patients aged 18 years or older with acute BTI. The NSC system was compared with the GCS in the BTI classification.
Results: Of 29 patients, 82.76% were male and 82.76% were between 18 and 64 years old. The severity of the TBI through the NSC System was very mild 6.70%, mild 17.24%, moderate 51.72%, severe 17.24%, and critical 6.70%. There was an association between the NSC System and the Rotterdam Computed Tomographic Score (RCTS) (p = 0.005), a moderate positive correlation of the NSC System with the RCTS (Rho 0.6773, p = 0.0001), an association between the NSC System and the indication for neurosurgical intervention (p = 0.002), as well as high sensitivity-specificity in the distinction of severity categories with the NSC System, and lower GCS performance.
Conclusions: The NSC clinical-tomographic system improves the determination of the severity of BTI in comparison with GCS and provides an excellent relationship with the indication for neurosurgical intervention.
Keywords: Brain Injuries, Traumatic, Brain, Glasgow Coma Scale, Functional Status (Source: MeSH NLM)
Presigmoid transpetrous approach (partial petrosectomy) combined with subtemporal transtentorial approach for petroclival meningioma
FERNANDO PALACIOS S., MANUEL LAZON A., EDUARDO ROMERO V., ROMMEL RODRIGUEZ B.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
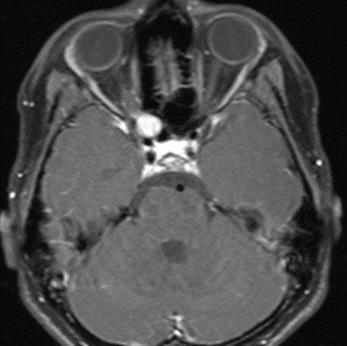
Introduction: Petroclival meningiomas constitute 3 to 10% of meningiomas of the posterior fossa, they originate in the petroclival fissure, in the upper part of the clivus, petrosal apex, and medial to the trigeminal nerve. Resection of these tumors is a neurosurgical challenge. The combined partial petrosectomy approach associated with a sub-temporal approach is a technique described by various authors; however, its performance is considered highly complex. We report the case of a petroclival meningioma operated successfully in our hospital using a combined presigmoid and subtemporal transtentorial transpetrosal approach.
Clinical case: 33-year-old female patient with a clinical picture of headache, nausea, and gait disturbance. Brain magnetic resonance imaging showed a large right petroclival tumor (4.2x3.9x3.8cm) that displaced the brainstem and secondary hydrocephalus. The hydrocephalus was treated with a ventricular peritoneal shunt. Then, the tumor was resected using a combined presigmoid and subtemporal transpetrosal approach, a technique that allowed adequate exposure of the tumor, achieving complete resection, without intraoperative complications. Postoperative evolution was favorable, with no sequelae.
Conclusion: The combined presigmoid and transtentorial subtemporal transpetrous approach for petroclival meningiomas is an effective and feasible technique to perform in our environment. The support of technology such as Neuronavigation, the ultrasonic aspirator, intraoperative monitoring, and adequate experience in skull base surgery are fundamental factors for the success of this surgery.
Keywords: Meningioma, Skull Base Neoplasms, Craniotomy, Neurosurgical Procedures. (Source: MeSH NLM)
Orbital schwannoma, a rare entity. case report
JOHN VARGAS U., CAMILO CONTRERAS C., FERNANDO PALACIOS S., EDUARDO ROMERO V.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Orbital schwannoma is a rare pathology, which constitutes approximately 1 to 6.5% of orbital tumors, and can originate from the ophthalmic branch of the 5th cranial nerve or from perioptic sympathetic nerves. Its diagnosis is made by magnetic resonance imaging (MRI) with contrast. The first-line treatment is surgery, and total resection provides a good prognosis. The time of illness is used to evaluate the visual prognosis in these patients.
Clinical Case: A 12-year-old woman, with a 9-year illness, characterized by a progressive decrease in right visual acuity until reaching amaurosis. Brain MRI with contrast shows an isointense tumor on T1, adhered to the medial aspect of the optic nerve sheath, which captures contrast, slightly hyperintense on T2. Total resection of the lesion is performed, and the diagnosis of schwannoma is confirmed by pathological anatomy. A month after surgery, the patient had slightly recovered her vision, without presenting other complications.
Conclusion: Orbital schwannoma is a rare pathology that must be treated surgically as soon as possible to achieve a better visual prognosis for the patient.
Keywords: Neurilemmoma, Optic Nerve, Orbital Neoplasms, Cranial Nerves, (source: MeSH NLM)
Double aneurysm clipping of true fetal posterior communicating artery by minipterional approach plus control with sodium fluorescein: a case report
CRISTIAN SALAZAR C., ALLEN DIAZ I., RICARDO ROJAS D., MIGUEL GAITAN C., ARMANDO LUCAR F.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
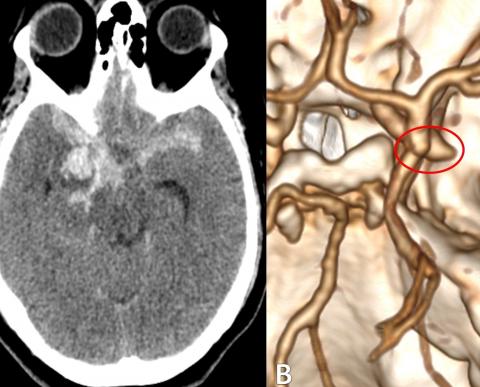
Introduction: True fetal or fetal type posterior communicating artery aneurysms (PComA) are a technical challenge for the neurosurgeon in both endovascular and microsurgical treatment. Microsurgical clipping using minimally invasive approaches is a safe and optimal alternative solution.
Clinical case: a 53-year-old patient who presented subarachnoid hemorrhage, Hunt & Hess scale III, Fisher scale III, and Glasgow Coma Scale of 13. Cerebral angioCT showed two saccular aneurysms in the right true fetal PComA. The patient underwent a right interfacial minipterional craniotomy and clipping of the 2 aneurysms, using sodium fluorescein as a guide. Total occlusion of the aneurysms was achieved, maintaining the patency of the fetal PComA.
Conclusion: The minipterional approach allows adequate access to the fetal PComA and the aneurysms originating from it. It is essential to review the patency of the adjacent vessels, being the use of intraoperative fluorescein is an essential complement to avoid complications such as cerebral infarction.
Keywords: Intracranial Aneurysm, Craniotomy, Fluorescein, Subarachnoid Hemorrhage, Neurosurgeons (Source: MeSH NLM)
Pneumocephalus and CSF leak secondary to skull base fracture by pyrotechnical object: case report
MARCOS VILCA A., CARLOS R. PALACIOS P., SOFIA ROSAS L., ERMITAÑO BAUTISTA C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Pneumocephalus is mainly associated with traumatic injuries, being a rare complication but with high mortality rates; it behaves like a space-occupying lesion and increases intracranial pressure. The symptoms are not specific, but in the event of trauma it is necessary to suspect this entity to carry out a timely diagnosis and treatment, since being the product of the skull base fracture it can cause communication with the outside, and the appearance of cerebrospinal fluid (CSF) leak.
Clinical Case: a 38-year-old male patient who suffers trauma from a pyrotechnic explosion near his right ear, when handling a pyrotechnic object (whistle) during the New Year, presenting severe pain, slight bleeding in the right ear, feeling faint and holocranial headache that increased in a standing position; likewise, he presents high-flow aqueous secretion (CSF) from the right ear. Brain and skull base tomography (CT) showed air in the intracranial cavity, fracture of the skull base, and the ossicles of the right middle ear. Conservative management was performed using rest and lumbar drainage, presenting a satisfactory evolution.
Conclusion: Pneumocephalus is a frequent and expected complication of trauma with a skull base fracture. Its early and timely diagnosis using skull base CT is essential to define therapeutic measures. Accidents due to the misuse of pyrotechnics continue to be a relevant problem in our country. Knowing and disseminating its consequences can help raise awareness in the population.
Keywords: Pneumocephalus, Skull Base, Intracranial Pressure, Cerebrospinal Fluid Leak. (Source: MeSH NLM)
Choroid plexus coagulation as an isolated procedure in the treatment of hydrocephalus
STEFANO SMOQUINA, S., JOSÉ MANUEL ZULUETA.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
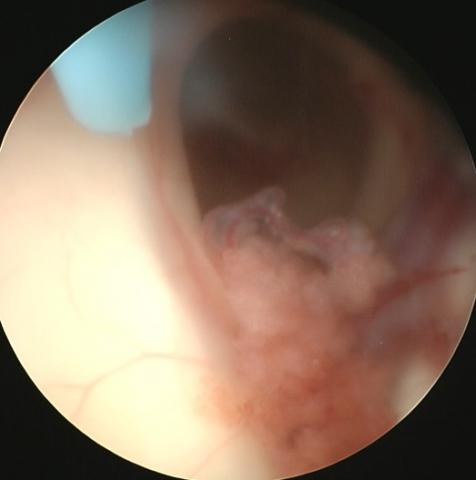
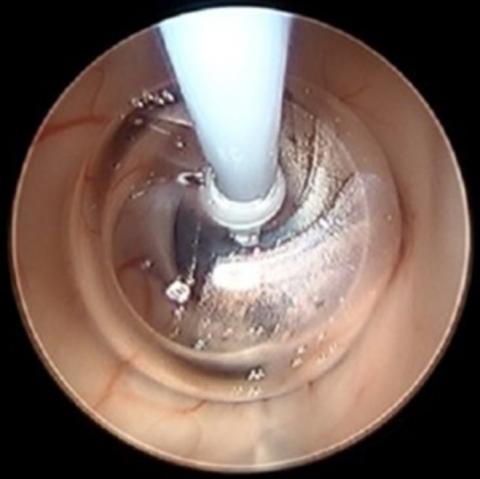
Objectives: The objective of this review is to determine the effectiveness of isolated choroid plexus coagulation (CPC) as a treatment for hydrocephalus in various clinical settings and the variables associated with its success.
Methods: PubMed was searched for the terms (choroid plexus coagulation) OR (choroid plexus cauterization). Those studies published since 1990 were included so that they were relevant to current clinical practice. All studies evaluating the efficacy of CPC as an isolated procedure for treating hydrocephalus were included.
Results: The etiology, approach, and degree of CPC were significantly associated with the effectiveness of the procedure. The greatest effectiveness was reported in patients with hydranencephaly or maximum hydrocephalus (68.9%, p = 0.001276), when a parietal approach was used (74.4%, p = 0.000604), and when the temporal horn plexus was included (64.7 %, p = 0.048068). Furthermore, a case of choroid plexus hyperplasia (CPH) treated effectively with CPC is described. On the other hand, the type of electrode (p = 0.4631), the type of endoscope (p = 0.0699), and the presence of a previous ventriculoperitoneal shunt (p = 0.3241) were not significantly associated with the effectiveness of CPC.
Conclusions: CPC is a viable treatment alternative in the management of hydranencephaly, CPH, and in selected cases of hydrocephalus without the aforementioned characteristics. However, studies are needed to compare CPC with shunt therapies before qualifying it as the first line of treatment.
Keywords: Choroid Plexus, Cautery, Hydrocephalus, Hydranencephaly, Ventriculoperitoneal Shunt. (source: MeSH NLM)
Prognostic factors of success of endoscopic third ventriculostomy with choroid plexus cauterization in the management of hydrocephalus: a narrative review
STEFANO SMOQUINA, S., JOSÉ MANUEL ZULUETA.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
|
Currently, endoscopic third ventriculostomy with choroid plexus coagulation (ETV / CPC) has been positioned as a reasonable alternative to cerebrospinal fluid (CSF) shunt in the treatment of hydrocephalus, both in developing countries and in non-limited settings of resources. The results show that the short-term outcomes strongly depend on the age of the patient at the time of the procedure, the etiology of the hydrocephalus, anatomical characteristics, and previous procedures. Other predictive factors include postoperative radiographic markers and surgical technique. Consequently, the selection of patients is essential when deciding on the use of this procedure. The objective of this review is to determine the association of prognostic factors with the effectiveness of ETV / CPC, to facilitate decision-making regarding the use of this procedure.
Keywords: Ventriculostomy, Choroid Plexus, Hydrocephalus, Cerebrospinal Fluid Shunts. (source: MeSH NLM)
|
Extradural minipterional approach in clipping of ruptured and unruptured complex aneurysms in the “Luis N. Saenz” PNP Hospital Complex: case report
CRISTIAN SALAZAR C, ALLEN DIAZ I, RICARDO ROJAS D, MIGUEL GAITAN C, ARMANDO LUCAR F.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: The complexity of an intracranial aneurysm is defined by its location, size, previous treatment, presence or absence of collateral circulation, intraluminal thrombus, or calcification of the aneurysm wall. The treatment of these aneurysms must be based on the balance between the associated risks and the benefit for the patient; Within microsurgical techniques, the extradural minipterional approach is described.
Clinical case: a 33-year-old female patient who presented headache, vomiting, and sensorial disorder, being diagnosed with 2 complex aneurysms, one in the ruptured ophthalmic segment and the other in the unruptured right pituitary. She underwent an extradural minipterional craniotomy plus aneurysm clipping with complete occlusion and a favorable outcome.
Conclusion: The knowledge of new microsurgical techniques in the management of complex cerebral aneurysms is crucial to obtain satisfactory results, being the extradural minipterional approach an alternative and key approach for the treatment of these lesions, which represent a challenge for the neurosurgeon.
Keywords: Intracranial Aneurysm, Craniotomy, Collateral Circulation, Neurosurgeons (Source: MeSH NLM)
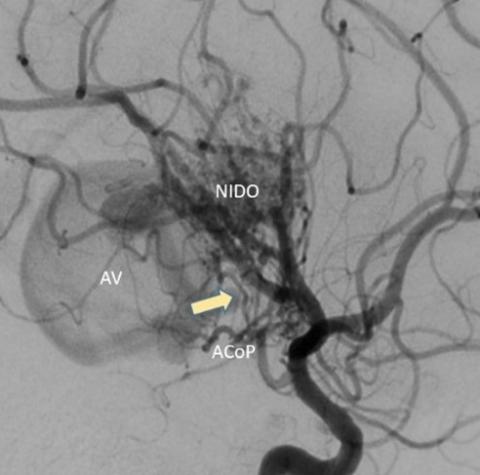
Experience of endovascular management of a unruptured thalamus-mesencephalic arteriovenous malformation associated with venous aneurysm in a pediatric patient. case report
ANNEL MURGA V., JESÚS FLORES Q., GIANCARLO SAAL Z., OSMAR ORDINOLA C., RODOLFO RODRÍGUEZ V.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: The treatment of arteriovenous malformations (AVMs) of the basal ganglia, the thalamus, and the insula is complex, due to the eloquence of the neural structures involved. They constitute between 4.3% and 11% of all AVMs and are associated with a high rate of morbidity and mortality due to the high risk of bleeding due to their inaccessible location Recent advances in endovascular therapy have allowed obtaining good results with curative potential.
Clinical case: 7-year-old male patient with headache, nausea, and left hemiparesis (Daniels 4/5). The cerebral tomography showed an unruptured thalamic-mesencephalic vascular lesion, with slight ventricular dilation due to partial collapse of the Monroe foramen. A brain angioCT showed an arteriovenous malformation with a large bilobed venous aneurysm with mass effect. Subtraction angiography revealed a right thalamic-midbrain AVM with afferents from perforating branches of P1, P2, and right PComA, the largest with a diameter of 0.88 mm, with a single thick venous drainage and a large venous aneurysm, reaching the internal cerebral vein already Galen's vein. It was embolized with Squid ® 4.5cc in a single session via the arterial route, with almost total occlusion (95%) of the nest, as well as the closure of the ostium to the efferent vein.
Conclusion: Embolization is a curative treatment strategy in selected cases of patients with deep AVMs, with good results and complication rates comparable to other therapeutic strategies.
Keywords: Arteriovenous Malformations, Embolization, Therapeutic, Basal Ganglia, Aneurysm (Source: MeSH NLM)
McCune Albright syndrome, craniofacial manifestations, and surgical treatment. pediatric case report
GABRIELA ESPIN O., ALICIA TORRES M., JESUS CASTRO V., RODOLFO BERNAL C.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: McCune-Albright syndrome (MAS) is a rare and complex genetic disease that affects the skin, skeleton, and endocrine system. The clinical triad described is composed of polyostotic fibrous bone dysplasia, café-au-lait skin pigmentation, and precocious puberty. When it is associated with myxoma, it is called Mazabraud's syndrome. The variable constellation of symptoms arises from a somatic activating mutation of the GNAS gene, which is present in many types of tissues.
Clinical Case: The case of a 6-year-old patient is presented, with a clinical presentation of a bone lesion in the left superciliary region with progressive growth for 10 months, suggestive of MAS. We focus on the course of the disease and neurosurgical treatment with the Neuronavigation technique, all carried out in our institution.
Conclusion: McCune Albright syndrome is an example of the genetic heterogeneity of polyostotic fibrous dysplasia, it is benign and has a low prevalence, with a great impact on quality of life, therefore treatment must be timely and multidisciplinary.
Keywords: Fibrous Dysplasia, Polyostotic, Puberty, Precocious, Craniofacial Fibrous Dysplasia (Source: MeSH NLM)
Bifrontal epidural hematoma. A case report at 3800 mamsl in Puno, Perú
SAMIR COLQUEHUANCA CH., LIZBETH CORA L., NATALI ABAD ILLACUTIPA M.
Abstract (Spanish) ||
Full Text ||
PDF (Spanish) ||
PDF (English)
ABSTRACT
Introduction: Epidural hematomas are one of the most frequent complications of head injuries. Bifrontal epidural hematomas (BEH) are rare, are associated with high-intensity trauma, and are associated with high mortality. We present the clinical case of a patient with bifrontal epidural hematoma with a Glasgow Coma Scale of 6/15 on admission.
Clinical case: A 27-year-old male patient suffered a traffic accident while riding a linear motorcycle without protection, in an apparent alcoholic state. He was diagnosed with a multifragmentary depressed skull fracture and a bifrontal epidural hematoma, which extended to the temporoparietal region of the right side with a volume greater than 215cc and with a high risk of nailing. A bifrontal craniotomy and evacuation of the epidural hematoma were performed. The postoperative evolution was favorable despite a mild neurological sequela.
Conclusion: Bifrontal epidural hematoma is a rare clinical entity, and its prognosis depends on the preoperative neurological situation.
Keywords: Hematoma, Epidural, Cranial, Craniocerebral Trauma, Craniotomy (Source: MeSH NLM)