Usted está aquí
Peruvian Journal of Neurosurgery
First experience using 5-ALA for high grade gliomas in the Almenara Hospital
ABSTRACT
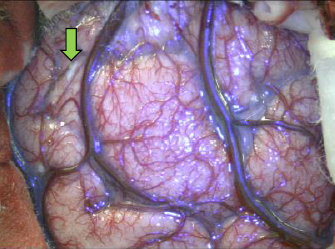
Introduction: The most frequent brain tumors in adults are high-grade gliomas and meningiomas. Having a discouraging prognosis of high-grade gliomas and knowing that the prognosis improves depending on the degree of tumor resection, is that new therapeutic strategies are sought, one of them is the use of 5-aminolevulinic acid (5-ALA) thanks to the fluorescence it produce in the tumor it allows to improve the rate of tumor resection, finally improving the prognosis of the patients. We presented the first experience in Almenara Hospital of the use of 5-ALA in a patient with a diagnosis of high-grade glioma.
Clinical Case: Presents itself the case of a 48-year-old male patient with clinical evidence of motor and sensory deficit contralateral to the lesion, without alteration of the state of consciousness. The magnetic resonance of the encephalon with contrast, a right frontal lesion is evidenced compatible with high-grade glioma. Therefore, it is programmed for guided surgery with fluorescence, where 5-ALA is used, and a total resection of the tumor is performed, obtaining an anaplastic ependymoma as pathological anatomy. The patient presented an increase in the motor deficit, which he later recovered. In the tomographic control with contrast at 4 months, complete tumor resection is evident.
Conclusion: 5-aminolevulinic acid is a drug that helps to properly delimit the edges of a high-grade glioma, by using a modified microscope, and thus increases the degree of tumor resection, ultimately improving the prognosis of the disease.
Keywords: Glioma, Aminolevulinic acid, Ependymoma, Fluorecense, Prognosis. (source: MeSH NLM)
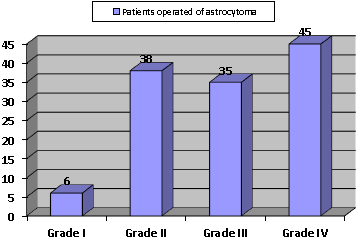
Prognostic factors in the survival of patients operated of astrocytoma grade II
ABSTRACT
Cerebral aneurysm diagnosed with angio-tomography and its surgical correlation at Daniel A. Carrión Hospital in the period May 2004 to November 2007
ABSTRACT
Objective: To determine the validity, sensitivity and specificity of multislice spiral CT angiography (ATEM) with a 16-Multislice CT scanner detector lines in the diagnosis of cerebral aneurysms and their most frequent localizations.
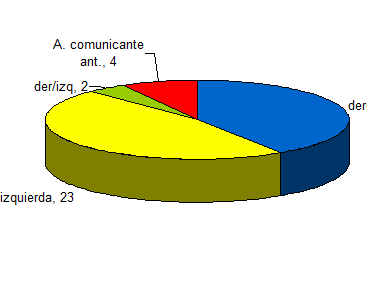
Patients and Methods: We selected 51 patients with nontraumatic subarachnoid hemorrhage due to suspected intracranial aneurysm who underwent surgery in the Hospital Daniel A. Carrión, Callao, for the period May 2004 to November 2007.
Results: The sensitivity of the ATEM for the detection of intracranial aneurysms in this study was 100%. The resulting specificity was 50%. The positive predictive value (PPV) of ATEM for the diagnosis of cerebral aneurysms was 98%, with 87.8% accuracy of the method for determining the location of the aneurysm and 12.2% of uncertainty in the determination of the location of this anomaly. The average size of the aneurysm at surgery was 11.33 + / - 6.9 mm. While the average size of the aneurysm by ATEM was 8.60 + / - 5.75 mm. The difference between the means of these measurements was significant (p = 0.027). 70.3% of aneurysms in this study were found in posterior communicating segment of both internal carotid and middle cerebral arteries both.
Conclusion: CT angiography is an excellent noninvasive test for the detection of intracranial aneurysms and to determine its location.
Key words: Intracranial aneurysm, CT Angio (ATEM), aneurysm surgery
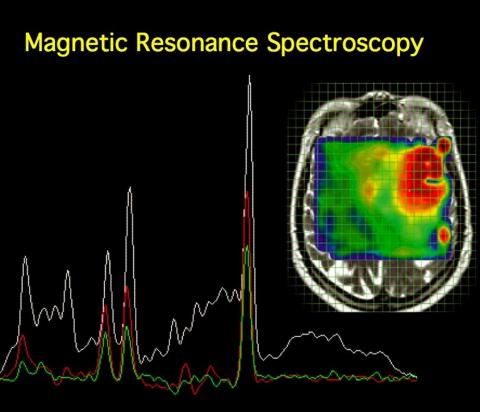
MRI Spectroscopy (H+) in the differential diagnosis between brain tuberculomas and intra-axial neoplastic process
ABSTRACT
Patients and Methods: A descriptive case series, 24 patients aged between 02 and 72 years who underwent the brain structural and spectroscopic study univoxel with voxel of 20 mm x 20 mm x 20 mm (8 cc ) located at the level of the lesion determined. Resonator was used 1.5-tesla General Electric Smart Speed and Hdx models. Ratios were assessed Choline / creatine, and N-Acetil-Aspartato/Creatina and Mio-inositol/Creatina. All cases were confirmed anatomical - pathological or therapeutic test.
Results: The ratio choline / creatine for intra-axial brain tumors was found to be 1.97 compared with tuberculomas which was 1.15, which is statistically significant (p = 0.017, Mann Whitney). Mio-inositol/creatina ratio for intra-axial brain tumors was 0.89 compared with tuberculomas was 0.55 which is statistically significant (p = 0.008, Mann Whitney). The ratio N-Acetil-Aspartato/Creatina for intra-axial brain tumors was 0.96 compared with tuberculomas was of 1.28 which is statistically significant (p = 0.003, Mann Whitney).
Conclusion: Magnetic resonance spectroscopy allows a more accurate diagnosis of intraparenchymal brain lesions of uncertain etiology and occurs when the lesion is unique, brain neoplasia and tuberculomas, enabling better-targeted treatment for patients.
Type IV spinal arteriovenous malformations
ABSTRACT
We present the case of a 32 year old patient with spinal cord compression syndrome of 10 months of evolution. Magnetic resonance imaging showed signal voids causing myelopathy that spinal angiography showed to be a type IVb spinal arteriovenous malformation (perimedular arteriovenous fistula type II) supplemented by a posterior spinal artery that originated next to the Adamkiewicz artery from the segmental artery T11 left. The fistula was successfully eradicated by transarterial embolization with cyanoacrylate and the patient experienced progressive improvement. The relevant literature is reviewed. The endovascular approach is the treatment of choice in spinal arteriovenous malformations types IVb and IVc.
Chronicle of the Department of Neurosurgery of Police Hospital
ABSTRACT
Neurosurgery is successively founder Mauricio Dávila in 1944 at the Police Hospital, Esteban Roca in 1947 in the Obrero Hospital, Fernando Cabieses at the Institute of Neoplastic Diseases and Juan Franco the the Institute of Neurological Sciences . After these services have made many more, led by prominent and prestigious Neurosurgeons meeting in what today is the Peruvian Society of Neurosurgery. The academic activity of the neurosurgeons was performed at baseline in 1938 in the Peruvian Society of Neuro-Psychiatry and Legal Medicine which was only shortly after Peruvian Society for Neuro-Psychiatry and when the number of neurosurgeons was higher is nominated Peruvian Society of Psychiatry, Neurology and Neurosurgery.
In 1961 he inaugurated a Police Hospital Central Pavilion and 4 plants with capacity of 500 beds and is given the name of the Central Police Hospital "General Luis N. Saenz. "Humberto Hinojosa travels to the U.S. for graduate studies with Irving Cooper Esterotaxia surgery, to return the Police Hospital becomes the first team in the country Esterotaxia surgery and allows many operations of this type.
Surgical Treatment of Traumatic brain injury: Results in a series of 76 patients
ABSTRACT
Objective: Traumatic brain injury (TBI) is the leading cause of morbidity and mortality mainly in young people, and also one of the most common neurosurgical diseases in daily practice. The surgical management is a fundamental part of TBI. The aim of this study is to present the results in 76 patients operated on at Almenara Hospital in 2008 and 2009.
Patients and Methods: We conducted a descriptive study of patients undergoing BTI during 2008 and 2009. We reviewed the medical records and operative reports, and pooled data on sex, age, disease duration, degree of BTI, location, type of medical management and use of ICP, type of surgery, hospital stay, GOS and Glasgow discharge, complications and mortality.
Results: 76 patients were operated of which 76% were male and 24% female. The most affected age group was 20-29 years (18.4%) followed by the under-10 years (15.8%). Patients admitted to hospital more frequently (38.3%) among 13-24, with moderate TBI most common grade (63.3%). Regarding treatment, the hypertonic solution was the most used in the ICP management, using intracranial pressure monitoring in 15.8% of cases. The patients were operated on by craniotomy (78.9%) and decompressive craniectomy (21.1%). The average Glasgow Coma Scale at admission increased from 10.9 to 14 at discharge, being higher in the EH and lower in contusion. The most common discharge GOS was V (36.8%) and IV (35.6%). The most common complication was pneumonia (27.6%) and overall mortality rate was 11.8% being higher (21%) in the ASDH.
Conclusions: The BTI treatment has evolved in recent years, the use of hypertonic solutions and intracranial pressure monitoring are essential in the medical management of moderate and severe TBI, the classic craniotomy is the cornerstone of surgical management but decompressive craniectomy being increasingly especially common in cerebral contusion. Medical and surgical optimal treatment are essential to achieving shorter hospital stay, good Glasgow scale and GOS, reduce complications and mortality rate.
Intracraneal Pressure Monitoring
ABSTRACT
Continuous monitoring of intracranial pressure (ICP) is a therapeutic guide for the proper management of Brain injured patients at risk of intracranial hypertension. Intracranial hypertension is associated with high morbidity and mortality in brain injury patients of different etiologies, hence the importance of timely recognize and treat this entity. For this reason the need for monitoring, analysis and interpretation of intracranial pathophysiological is an important part of multimodal neuromonitoring, which together with clinical and CT evaluation. The integration of neuromonitoring is fundamental and has a great impact on the outcome of brain injury patients and is essential for proper therapeutic management.
Intraoperative Intracraneal pressure monitoring in decompressive craniectomy for severe TCE
ABSTRACT
The reduction of intracranial pressure (ICP) is a cornerstone in the management of patients with severe head injury, ICP monitoring remains very important as it helps to optimize treatment and improve prognosis. Decompressive craniectomy (DC) has proved to be an effective method in reducing intracranial pressure when other treatments have failed. ICP monitoring studies in the pre and post operative show that this reduction is immediate and sustained within 48 hours. However, little is known about the variation of the ICP during the performance of decompressive craniectomy and the contribution of each of its stages, as the removal of bone, dural opening and duraplasty in the final result. We report the case of a patient with severe TBI who underwent intracranial pressure monitoring during the performance of decompressive craniectomy in the Guillermo Almenara Hospital in 2009.
Surgical treatment of cerebral radiation necrosis complicating stereotactic radiosurgery in skull base meningioma
ABSTRACT
Although stereotactic radiosurgery has been proven to be an effective and noninvasive treatment for some skull base meningiomas, complications such as swelling, radiation necrosis, and cranial nerve dysfunction are possible in some cases. As to date, a surgical treatment for radiation necrosis (induced by stereotactic radiosurgery) in order to treat skull base meningioma has yet to be reported in few cases. Due to corticosteroid intolerance we performed in one patient a surgical resection of the radiation necrosis and tumor. Albeit rare, clinicians referring patients for stereotactic radiosurgery must be aware of such complications.
Decompressive Craniectomy in the Management of Refractory PostTraumatic Intracranial Hypertension
ABSTRACT
Objective: Traumatic intracranial hypertension is the major pathophysiological issue of traumatic brain injury and its treatment usually demands general and specific measures; nevertheless decompressive craniectomy is an extreme resource available for refractory cases, current data are not enough to define its indications and long term results.
Patients and Methods: This study evaluates a cohort of 32 patients with refractory traumatic intracranial hypertension submitted to decompressive craniectomy as a randomized method of treatment between 2004 and 2008.
Results: The most remarkable characteristics of the procedure were: execution period < 72 hours, wide and extensive bone platelet, and complete specific surgical technique (craniectomy + durotomy / duroplasty ± resection/evacuation); whereas the most relevant results demonstrated: reduction of the ICP value in a great proportion of patients, short period of time until normalization of the ICP and lower hospitalization period at the Neurosurgical ICU, with an index of complications close to 34% (mainly early) and rate of mortality about 18% (mainly neurological). Functional prognosis was favorable at discharge in 25% and at 6 months in 54%, with a quality of life defined as independent or low dependency.
Conclusion: Although traumatic intracranial hypertension has a heterogeneous course, descompressive craniectomy is a useful option for its control and a better outcome of the traumatic brain injury in the long term.
Early results of cervical artroplaty using Prodisc-C
ABSTRACT
Objective: The use of an artificial cervical disc is a new technique that can replace the classical discectomy and fusion for lesion in the lower cervical spine. The purpose of this design is to reproduce the function of the intervertebral disc.
Patients and Methods: Between July 2004 and June 2007, 35 cervical arthroplasties were performed at Clinica Guemes, Lujan. 27 patients underwent a single or double disc replacement. The average age was 4A\]3.4 years (range 28-54). The patients were evaluated 45, 90, 180 and 365 days after surgery. The patients were evaluated using Neck Disability Index (NDI) and Visual Analogic Scale (VAS).
Results: A steady improvement could be observed in all patients tested by both scales.
Conclusion: The use of ProDisc-C in young patients appear to be an excellent option for the treatment of cervical disc herniation.
Benefits of the Spinal anesthesia in Surgery of Disc Herniation
ABSTRACT
Among the symptoms that most affect the man, for sure the pain is more frequent, and by far the most important. It jeopardizes the quality of life the daily activities and hence their productivity. The disc protrusion, is among the diseases that have this symptom, as the main complication. So it is to bring medical relief to the patient. You should immediately try a treatment, and when you do not get resolution with this conduct, it is for surgery.
Objective: It is exactly these patients with surgical indication, to demonstrate a broad casuist (2000 cases), the advantages of spinal anesthesia when anesthetic induction in compitum general, with regard the outcome. So that we can bring a greater contribution to those who
suffer this nosology.
Patients and Methods: In our series, the study included patients who had surgical treatment, with clinical diagnosis and through examination of images of disc herniation, and who agreed to participate in the study, which excluded only those who did not wish to participate in the study. The follow-up
from each patient and compared with data available in the literature so that we could see the gravy of our work.
Results: showed to be extremely favorable with regard to postoperative pain, a good development (99.72% of cases), only two patients had fistulas (0.11%), two cases had infection (0.11% ) and one had to go for general surgery in Trendelenburg position, inappropriate (0.06%).
Conclusion: Therefore it is concluded that this is an aspect that should be exploited by those who take care of this condition, the major advantages of this measure.
Schwannoma of the cauda equina causing low back pain and bilateral crural paraparesis
ABSTRACT
Neuromas, neurinomas, or neurilemmomas are benign tumors of peripheral nervous system, which have Schwann cell origin. Typically, schwannomas are typically solitary, ovoid or spindle, as well encapsulated and found along the peripheral nerves or surrounded by them. The location of the tumor is prevalent in the cervical and thoracic, and less frequent in the lumbosacral spine Moreover, growth has dragged normally are not aggressive, not malignant and are subject to cure by surgery. The attempt to separate the tumor from its adjacent nerve is often successful, leading to a preservation of neural function. Patient 48 years, history of low back pain radiating to lower limbs, which worsened when performing the Valsalva maneuver. On physical examination it was found paraparesis, hypotonia and hyporeflexia in both lower limbs. The same bore resonance that showed strong and heterogeneous lesion predominantly located at the first lumbar vertebra in topography intradural, extramedullary, which has received too heterogeneous enhancement by Gadolinium. Patient underwent laminectomy involving the twelfth thoracic and first lumbar vertebra. The tumor assumed ellipsoid shape, was attached to a thin nervous from the cauda equina, this being duly resected. After the procedure has evolved in the same manner satisfactory recovery of neurological function. The complexity of the case and the presence of atypical schwannoma of cauda equina call attention in this case.
Clinical and Epidemiological Characteristics of Patients with Hydrocephalus Secondary to Subarachnoid Hemorrhage Hospitalized in the Neurosurgery Department of Rebagliati Hospital 2007-2008
ABSTRACT
Objective: The aim of this study is to know the clinical and epidemiological characteristic of patients with hydrocephalus secondary to subarachnoid hemorrhage during the period April 2007-2008. There is no a complete knowledge about this pathology in our country.
Patients and Methods: We reviewed medical records of 110 patients who underwent surgical clipping of cerebral aneurysm. Of these we selected those who developed hydrocephalus secondary to subarachnoid hemorrhage and placed ventricle-peritoneal shunts corresponding to 23 patients .
Results: It was found that the hydrocephalus secondary to subarachnoid hemorrhage with a 43% of cases. It was found that the hydrocephalus secondary to subarachnoid hemorrhage occurred in 21% and most often from first to second month of the event of a subarachnoid hemorrhage with a 43 % of cases . Besides is more frequent in women over 50 years and disturbance of consciousness is the main clinical sintomatolgy . These findings are consistent with Anglo-Saxon literature available.
Conclusion: Surely a judicious indication of a VPS greatly influences the patient's recovery. However, it should be noted that the recovery of patients with subarachnoid hemorrhage is multifactorial.